Across North America, more parents are turning to melatonin to help their children fall asleep. It is widely available over the counter and often perceived as “natural” and therefore harmless. However, new high-quality evidence published in JAMA highlights an important reality: for most young children with typical neurological development, there is limited evidence that melatonin provides meaningful long-term benefit, and there are growing safety concerns.
A recent systematic review of 19 studies examining melatonin use in children aged 6 years and under found that while melatonin can help with sleep onset in certain specific situations—such as in children with autism spectrum disorder or other neurodevelopmental conditions—evidence is lacking for routine use in otherwise healthy children. Even more concerning, melatonin has become a leading cause of pediatric emergency department visits due to accidental ingestions and overdoses, with cases rising steadily over the past decade.
Why this matters for families
Many sleep difficulties in young children are behavioural and environmental rather than medical. Irregular bedtimes, stimulating screen use before bed, inconsistent routines, and parental sleep associations are common contributors. In these cases, medication is often not the most effective first-line solution.
The evidence strongly supports non-pharmacological sleep hygiene strategies, including:
- A consistent bedtime and wake time every day
- A predictable, calming bedtime routine
- Avoiding screens and bright light before bed
- Creating a dark, quiet, and cool sleep environment
- Encouraging children to fall asleep independently
These approaches address the root causes of most childhood sleep-onset problems and avoid the risks associated with unnecessary medication exposure.
When might melatonin be appropriate?
For selected children with clearly defined neurodevelopmental or circadian rhythm disorders, short-term melatonin use may be reasonable under medical supervision. However, even in these cases:
- Optimal dosing is not well standardized
- Long-term safety data are limited
- Ongoing monitoring is essential
This is not a supplement that should be started casually, continued indefinitely, or dosed by trial and error.
The role of pharmacists in safe, evidence-based care
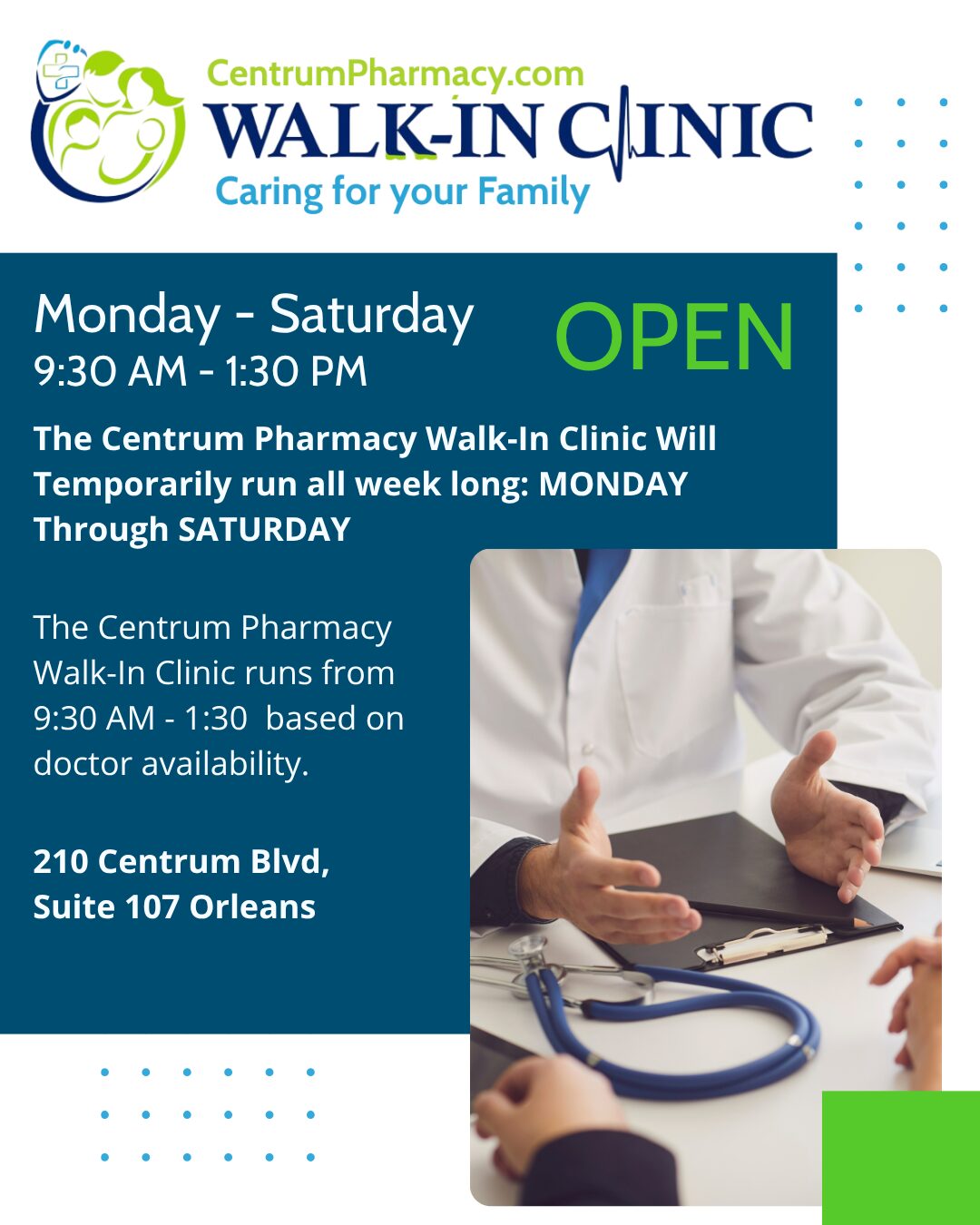
Uncontrolled retail or online purchasing of sleep supplements often bypasses proper clinical assessment. At Centrum Pharmacy, our pharmacist-led minor ailment care model ensures that every sleep concern is approached systematically and safely.
Our pharmacists are trained to:
- Assess whether a child’s sleep issue is behavioural, developmental, or potentially medical.
- Screen for red flags that require physician evaluation.
- Provide structured, evidence-based sleep hygiene counselling.
- Determine when medication might be appropriate and when it should be avoided.
- Coordinate directly with family physicians when follow-up or prescription therapy is needed.
This is part of our Complete, Comprehensive, Caring, and Connected Care (the “4 C’s”) approach:
- Complete: We evaluate the whole clinical picture, not just the symptom of “trouble sleeping.”
- Comprehensive: We provide both non-drug and drug options, prioritizing the safest effective strategy.
- Caring: We take the time to educate parents and tailor plans to each family.
- Connected: Through our integration with Orleans Family Health Clinic and our unmatched physician recruitment efforts, we can rapidly connect patients to a rostered family doctor when ongoing medical care is required.
Many families who visit Centrum Pharmacy for minor ailments or medication advice are successfully rostered with a family physician through this integrated model, ensuring continuity of care rather than fragmented, one-off advice.
Practical guidance for parents
Before reaching for melatonin:
- Speak with a pharmacist for an in-depth sleep assessment.
- Implement structured behavioural sleep strategies consistently for several weeks.
- Use medication only if there is a clear, evidence-based indication and a defined plan for monitoring and discontinuation.
If melatonin is used, it should be:
- At the lowest effective dose
- Stored securely to prevent accidental ingestion
- Regularly reassessed with a healthcare professional
The bottom line
Melatonin is not a harmless universal sleep aid for children. For most young kids, better sleep comes from better routines, not pills. When sleep problems persist, pharmacist-led counselling combined with seamless access to family physicians provides a safer, smarter path forward.
At Centrum Pharmacy, our integrated, pharmacist-physician model ensures that families receive expert, evidence-based guidance while remaining connected to comprehensive primary care.
If your child is struggling with sleep, book a minor ailment consultation with our pharmacists today and let us help you build a safe, effective plan.
Stay Connected with Centrum Pharmacy!
If you found this article helpful, don’t forget to like, share, and Follow to stay up to date on our latest health tips, pharmacy updates, and wellness advice.
Come for the Convenience, Stay for the Service.
Caring for Your Family Since 1999
Disclaimer: The medical information on this site is provided as an information resource only and is not to be used or relied on for any diagnostic or treatment purposes. This information does not substitute for professional diagnosis and treatment. Please do not initiate, modify, or discontinue any treatment, medication, or supplement solely based on this information. Always seek the advice of your healthcare provider first. Full Disclaimer.