That uncomfortable burning sensation after a meal? You’re definitely not alone. Heartburn, often a symptom of acid reflux, is a common complaint, and it seems to be on the rise for many Canadians. If you’ve ever found yourself reaching for an antacid after dinner, you’re part of a significant group. That familiar sour taste and the uncomfortable sensation of stomach contents rising into the throat are hallmarks of acid reflux. While occasional heartburn is common, persistent symptoms can significantly impact quality of life and may indicate a more chronic issue.
What Are the Symptoms of Acid Reflux?
Acid reflux can feel different for everyone, but the symptoms are often uncomfortable and disruptive. Recognizing them early is key to finding relief and preventing long-term complications.
Common acid reflux symptoms include:
- Heartburn: A burning sensation in the chest, often after eating or when lying down.
- Regurgitation: A sour or bitter-tasting acid backing up into your throat or mouth.
- Chest discomfort: Sometimes mistaken for heart-related pain, especially after meals.
- Chronic cough or sore throat: Caused by acid irritating the throat.
- Hoarseness or voice changes: Especially noticeable in the morning.
- Difficulty swallowing (dysphagia): A sensation that food is stuck or slow to move down.
- Bloating and belching: From swallowed air or acid disturbance in the stomach.
Not everyone experiences all symptoms, and some people may only experience symptoms like chronic cough or throat irritation, without classic heartburn. If you’re noticing any of these signs regularly, it’s time to speak to a healthcare professional.
What Causes Acid Reflux and Why is it So Common?
Several factors contribute to the prevalence of acid reflux. Rising rates of obesity are a significant concern. Excess body weight, particularly around the abdomen, can increase pressure on the stomach, making it easier for stomach acid to flow upwards into the esophagus.
However, weight isn’t the only culprit. Certain lifestyle choices and conditions can also cause or worsen acid reflux:
- Dietary Triggers: Spicy, fatty, or acidic foods, as well as large meals, can be problematic for some individuals.
- Smoking: Smoking can weaken the lower esophageal sphincter (LES), the muscle that normally prevents acid from leaving the stomach.
- Excessive Alcohol Consumption: Alcohol can also relax the LES and irritate the esophagus.
- Hiatus Hernia: This condition occurs when part of the stomach pushes upward through an opening in the diaphragm, which can impair the normal barrier against reflux.
- Pregnancy: Hormonal changes and the physical pressure of a growing baby make pregnant individuals more susceptible to heartburn.
Is Acid Reflux Dangerous? – The Importance of Managing Acid Reflux
It’s crucial to take acid reflux seriously. Repeated exposure of the esophagus to stomach acid can be dangerous and lead to damage over time. This may result in complications such as Barrett’s esophagus, a condition where the cells lining the esophagus change, potentially increasing the risk of esophageal cancer. According to gastroenterology specialists, while medications can be very effective in controlling symptoms and are generally well-tolerated, the goal is always to use the lowest effective dose for the shortest possible time.
Acid Reflux Medication – Understanding Your Treatment Options
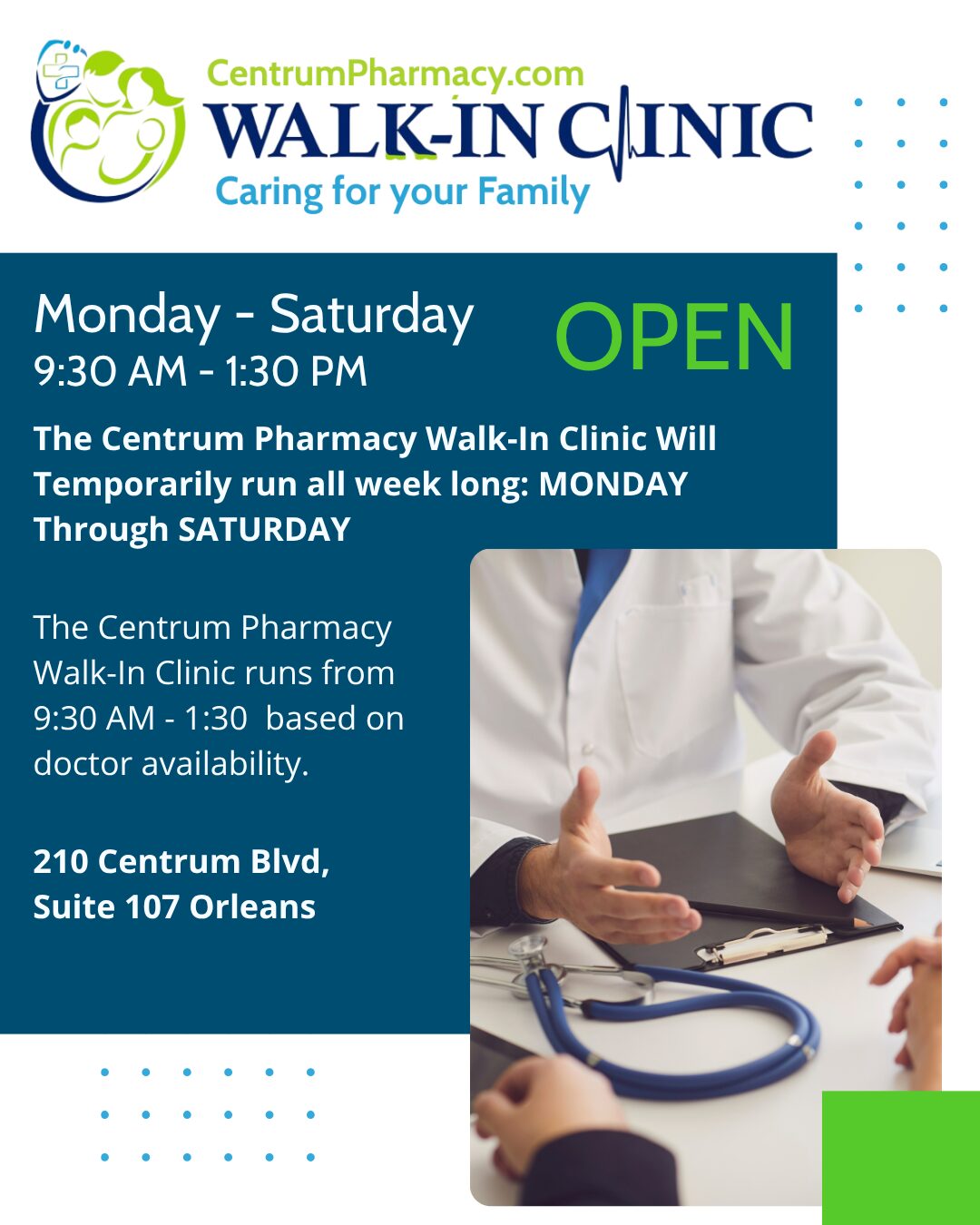
If you’re struggling with acid reflux, several treatment options are available, from over-the-counter remedies to prescription medications. Did you know your pharmacist can now assess and prescribe for acid reflux and other minor ailments in Ontario? If you’re dealing with persistent symptoms or aren’t sure which treatment is right for you, skip the wait and talk to us today.
1. Antacids
Readily available in pharmacies and supermarkets across Canada, brands like Tums, Rolaids, Gaviscon, and Pepto-Bismol are common choices for quick relief. Antacids work by neutralizing stomach acid or by creating a protective barrier that coats the esophagus. They offer the advantage of near-immediate effect and are generally considered safe for most people for occasional use.
However, it’s important to remember that antacids don’t address the underlying cause of excess acid production or why it’s refluxing. Long-term or excessive use can lead to side effects due to their mineral content. For instance, some antacids containing magnesium can cause diarrhea, while those with aluminum or calcium might lead to constipation. Electrolyte imbalances or mineral overload are potential concerns with prolonged, high-dose use.
Lifestyle adjustments, such as dietary changes, avoiding smoking, and moderating alcohol intake, should always be discussed with your doctor or pharmacist. These changes can potentially reduce the need for long-term antacid use.
2. H2 Blockers (Histamine H2-receptor antagonists)
Introduced in the 1970s, H2 blockers like famotidine (Pepcid) work by reducing the amount of acid your stomach produces. Research suggests they are effective for a significant percentage of acid reflux cases.
While generally considered safe, and perhaps a better option than PPIs for long-term use in some cases, H2 blockers aren’t without potential issues. They can interact with other medications because they affect stomach acid levels, which can influence the absorption of drugs that require an acidic environment. For example, some H2 blockers can affect how blood thinners work or alter the clearance rates of other medications. It’s crucial to discuss all current medications with your pharmacist before starting an H2 blocker.
3. PPIs (Proton Pump Inhibitors)
Proton Pump Inhibitors, such as omeprazole (Losec) and esomeprazole (Nexium), are highly effective in reducing stomach acid production, often successfully managing symptoms in about 90% of cases. They work by targeting the enzyme activity responsible for acid production in the stomach lining, which reduces irritation and allows the esophagus to heal.
However, for individuals with severe or chronic acid reflux, PPIs might be prescribed for extended periods – sometimes years or even decades. While generally safe, long-term use has been linked in epidemiological studies to a range of potential health issues. These include a slightly increased risk of osteoporosis (possibly due to effects on calcium absorption), vitamin B12 and magnesium deficiencies (as stomach acid aids in their absorption), kidney problems, and disruptions to the gut microbiome, which could increase the risk of certain infections like Clostridium difficile.
Because of these potential risks, regular review is often recommended for those on long-term PPIs, especially for milder conditions. This might involve attempting to taper off the PPI, possibly switching to an H2 blocker, and then to an antacid as needed. Gradual weaning can help individuals potentially discontinue these medications and avoid long-term complications.
It’s important to note that for some individuals with severe conditions like Barrett’s esophagus or significant inflammation of the esophagus, long-term PPI use may be necessary and the benefits may outweigh the risks. Often, patients on long-term PPIs have other underlying health conditions, which can also contribute to some of the observed health problems.
Can You Become Dependent on Acid Reflux Medications?
A phenomenon known as “rebound acid hypersecretion” can occur with all types of acid reflux medications. This is when stopping the medication leads to an increase in acid production and a worsening of reflux symptoms. This can often be managed by gradually tapering off the medication – reducing the dosage or frequency slowly over time – rather than stopping abruptly.
What’s on the Horizon for Acid Reflux Treatment?
Gastroenterology specialists are optimistic about new treatment options emerging.
- Potassium-Competitive Acid Blockers (P-CABs): These are a newer class of drugs that are not yet widely available in Canada but are used in other parts of the world. Some research suggests P-CABs may be even more effective than PPIs for severe acid reflux and could offer an improved long-term safety profile. Their availability in Canada will be something to watch for in the coming years.
- Minimally Invasive Therapies: Endoscopic procedures are also becoming an alternative to long-term medication for some patients. These procedures, some of which use radiofrequency energy, aim to strengthen the muscle (the lower esophageal sphincter) that prevents stomach acid from flowing back into the esophagus. These options require careful discussion with a specialist and further testing, but they hold the potential to reduce or even eliminate the need for medication.
When to See Your Doctor
While occasional heartburn can often be managed with over-the-counter remedies and lifestyle adjustments, it’s important to consult your doctor if you experience:
- Frequent or severe heartburn (two or more times a week)
- Difficulty swallowing
- Persistent nausea or vomiting
- Unexplained weight loss
- Chest pain (especially if you’re unsure if it’s heartburn or something more serious)
- Symptoms that aren’t relieved by over-the-counter medications
Your doctor can help determine the cause of your symptoms, rule out more serious conditions, and recommend the most appropriate treatment plan for you. Living with persistent acid reflux doesn’t have to be the norm. With the right approach and medical guidance, you can find relief and protect your long-term health. Talk to your knowledgeable Centrum Pharmacist if you are experiencing heartburn symptoms.
Disclaimer: The medical information on this site is provided as an information resource only and is not to be used or relied on for any diagnostic or treatment purposes. This information does not substitute for professional diagnosis and treatment. Please do not initiate, modify, or discontinue any treatment, medication, or supplement solely based on this information. Always seek the advice of your healthcare provider first. Full Disclaimer.