In Part 1 of our series, we explained how insurers are limiting pharmacy choice through patient steering. Now, let’s look at a real-world example: patients prescribed GLP-1 medications (such as Ozempic, Wegovy, or Mounjaro) for diabetes or weight management.
Insurers increasingly restrict coverage for GLP-1s to Preferred Provider Network (PPN) pharmacies. Here’s what that means for patients:
- Delays in access: GLP-1 supply is already tight. Being forced to use a PPN pharmacy only makes things worse.
- Confusion & miscommunication: Switching between pharmacy systems creates errors and missed follow-ups.
- Weaker monitoring: GLP-1s require close follow-up for nausea, gastrointestinal side effects, and blood sugar control. Insurer-owned pharmacies don’t coordinate with your doctor the way we do.
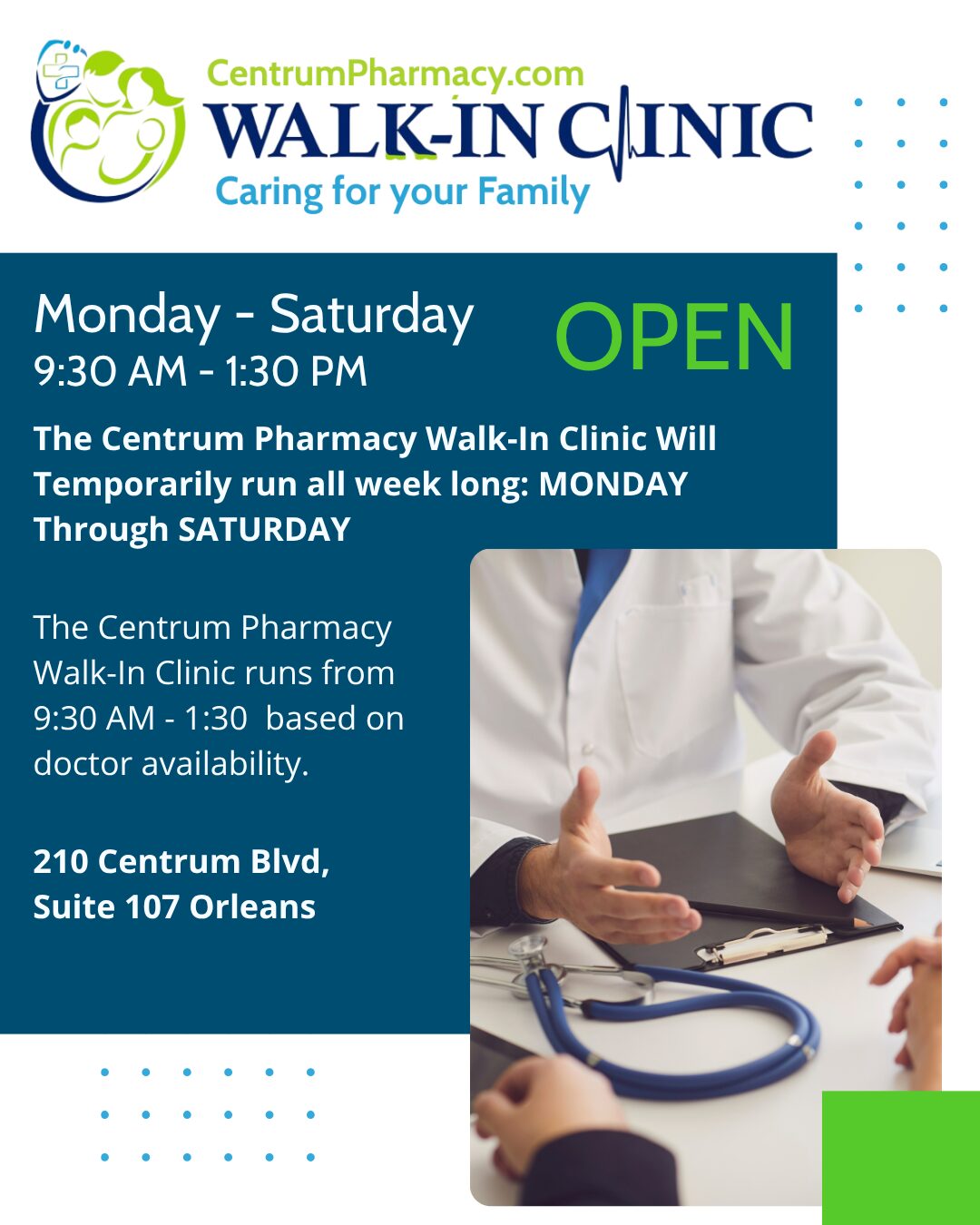
At Centrum Pharmacy, our integrated care model means we work directly with your family physician, monitoring your GLP-1 treatment for safety and effectiveness. That’s what Complete, Comprehensive, Caring, Connected Care looks like.
This is Part 2 of our series on insurer overreach. In Part 3, we’ll show why these aren’t isolated incidents — but a troubling pattern of behaviour across the industry.
Stay Connected with Centrum Pharmacy!
If you found this article helpful, don’t forget to like, share, and Follow to stay up to date on our latest health tips, pharmacy updates, and wellness advice.
Come for the Convenience, Stay for the Service.
Caring for Your Family Since 1999
Disclaimer: The medical information on this site is provided as an information resource only and is not to be used or relied on for any diagnostic or treatment purposes. This information does not substitute for professional diagnosis and treatment. Please do not initiate, modify, or discontinue any treatment, medication, or supplement solely based on this information. Always seek the advice of your healthcare provider first. Full Disclaimer.